Benign prostatic hyperplasia
Highlights
Benign Prostatic Hyperplasia (BPH)
Benign prostatic hyperplasia (BPH) is a condition in which the prostate gland becomes enlarged. However, the actual size of the gland does not necessarily predict symptom severity. Some men with minimally enlarged prostate glands may experience symptoms while other men with much larger glands may have few symptoms. BPH is very common among older men, affecting about 60% of men over age 60 and 80% of men over age 80.
BPH Symptoms
The symptoms associated with BPH are collectively called lower urinary tract symptoms (LUTS). These are generally classified as either voiding (obstructive) symptoms or storage (irritative) symptoms.
Common symptoms of BPH include:
- An urgent need to urinate and difficulty postponing urination
- A hesitation before urine flow starts despite the urgency to urinate
- Straining when urinating
- Weak or intermittent urinary stream
- A sense that the bladder has not emptied completely
- Dribbling at the end of urination or leakage afterward
Urinary retention (inability to void) is a serious symptom of severe BPH that requires immediate medical attention.
Treatment
BPH is not a cancerous or precancerous condition. It rarely causes serious complications, and men usually have a choice whether to treat it immediately or delay treatment. Treatment options include medications and surgery. Five-alpha-reductase inhibitors (5-ARIs) and alpha-blockers are the main types of drugs used for BPH treatment.
Drug Warning
- In 2011, the Food and Drug Administration (FDA) announced it had revised the prescription labels of 5-ARI drugs to include new information on increased risk of high-grade prostate cancer. Finasteride (Proscar, generic) and dutasteride (Avodart, Jalyn) are the 5-ARIs used for treating BPH. The FDA recommends that doctors rule out other urologic conditions, including prostate cancer, that may mimic BPH before prescribing 5-ARIs for BPH treatment.
- In 2012, the FDA revised the finasteride label to include the warning that sexual side effects (lowered libido, ejaculation disorders, orgasm disorders, and erectile dysfunction) may persist even after the drug is stopped.
Drug Approval
In 2011, the FDA approved the widely used erectile dysfunction drug, tadalafil (Cialis) for treatment of BPH. Tadalafil may be used to treat BPH and erectile dysfunction in men who have both conditions. Tadalafil should not be used in combination with alpha-blockers or nitrate drugs.
Introduction
Hyperplasia is a general medical term referring to an abnormal increase in cells. Benign prostatic hyperplasia (BPH) is noncancerous cell growth of the prostate gland. It is the most common noncancerous form of cell growth in men and usually begins with microscopic nodules in younger men. BPH is not a precancerous condition and does not lead to prostate cancer.
As BPH progresses, it can lead to enlargement of the prostate gland. About half of men with BPH go on to develop an actual overall increase in the size of the prostate. As BPH progresses, it can squeeze the urinary tube (urethra), causing urinary symptoms. These urinary difficulties are part of a group of symptoms called collectively lower urinary tract symptoms (LUTS).
About a third of men with BPH have LUTS symptoms that interfere with their quality of life. The size of the prostate gland does not necessarily relate to a patient’s symptoms. Not all men with BPH have LUTS, and not all men with LUTS have BPH.
The Prostate Gland
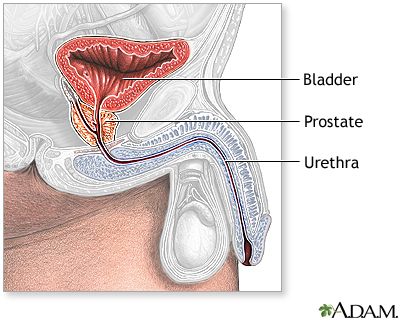
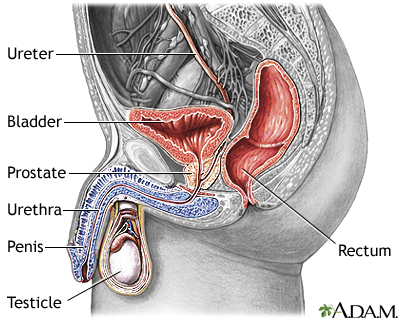
Description of the Prostate Gland. The prostate is a walnut-shaped gland located below the bladder and in front of the rectum. It wraps around the urethra (the tube that carries urine through the penis).
Functions of the Prostate Gland. The prostate gland provides the following functions:
- The glandular cells produce a milky fluid. During ejaculation, the smooth muscles contract and squeeze this fluid into the urethra. Here, it mixes with sperm and other fluids to make semen.
- The prostate gland also contains an enzyme called 5 alpha-reductase that converts testosterone to dihydrotestosterone, another male hormone with a major impact on the prostate.
Changes During the Lifespan. The prostate gland undergoes many changes during the course of a man's life. At birth, the prostate is about the size of a pea. It grows only slightly until puberty, when it begins to enlarge rapidly. It reaches normal adult size and shape, about that of a walnut, when a man is in his early 20s. The gland generally remains stable until about the mid-40s, when, in most men, the prostate begins to grow again through a process of cell multiplication (hyperplasia).
The Process of Urination
The process of urination is complicated:
- It begins when waste fluids flow out of the kidneys into two long tubes called ureters.
- The ureters empty into the bladder, which rests on top of the pelvic floor, a muscular structure similar to a sling running between the pubic bone and the base of the spine.
- The brain regulates muscles in the urinary tract through a pathway of nerves. As the bladder fills to its capacity of 8 - 16 oz of fluid, the nerves send signals from the bladder to the brain that indicate how full the bladder is.
- As the bladder fills, the outlet muscles contract to prevent urination.
- At the time of urination, the spinal cord initiates the voiding reflex. The detrusor muscle (which surrounds the bladder) contracts, while the internal sphincter (a strong muscle encircling the neck of the bladder) relaxes.
- When the internal sphincter is open, urine flows out of the bladder into the urethra (the tube that carries urine from the bladder out through the penis).
Causes
Doctors are not exactly sure what causes benign prostatic hyperplasia. The changes that occur with male sex hormone as part of the aging process appear to play a role in the enlargement of the prostate gland.
Male Hormones. Androgens (male hormones) affect prostate growth. The most important androgen is testosterone, which is produced in the testes throughout a man's lifetime. The prostate converts testosterone to another powerful androgen, dihydrotestosterone (DHT).
DHT stimulates cell growth in the tissue that lines the prostate gland (the glandular epithelium) and is the major cause of the rapid prostate enlargement that occurs between puberty and young adulthood. DHT is a prime suspect in prostate enlargement in later adulthood.
Female Hormones. The female hormone estrogen may also play a role in BPH. (Some estrogen is always present in men.) As men age, testosterone levels drop, and the proportion of estrogen increases, possibly triggering prostate growth.
Risk Factors
Age
Age is the major risk factor for BPH. Over half of men develop BPH by age 60 and about 85% of men have BPH by age 85. It is uncommon for BPH to cause symptoms before age 40.
Family History
A family history of BPH appears to increase a man's chance of developing the condition.
Heart Disease Risk Factors and BPH
Some evidence indicates that the same risk factors associated with heart disease may increase the risk of developing BPH. These risk factors include obesity, high blood pressure, low levels of HDL (“good”) cholesterol, diabetes, and peripheral artery disease (PAD). Lifestyle factors that are unhealthy for the heart (such as lack of physical activity, cigarette smoking, and poor diet) may also possibly increase BPH risk or worsen its symptoms.
Symptoms
Lower urinary tract symptoms (LUTS) are categorized either as voiding (formerly called obstructive) or storage (formerly called irritative) symptoms. BPH is often, but not always, the cause of LUTS, especially the voiding symptoms. Other medical conditions, such as bladder problems, can also cause these symptoms.
Some men with BPH may have few or no symptoms. The size of the prostate does not determine symptom severity. An enlarged prostate may be accompanied by few symptoms, while severe LUTS may be present with normal or even small prostates.
Voiding (Obstructive) Symptoms
Voiding symptoms can be caused by an obstruction in the urinary tract, which may be due to BPH. (Obstruction is the most serious complication of BPH and requires medical attention.) Voiding symptoms include:
- A hesitation before urine flow starts despite the urgency to urinate
- Straining when urinating
- Weak or intermittent urinary stream
- A sense that the bladder has not emptied completely
- Dribbling at the end of urination or leakage afterward
Storage (Irritative) Symptoms
Storage symptoms, also referred to as filling symptoms, include:
- An increased frequency of urination (every few hours)
- An urgent need to urinate and difficulty postponing urination
- Painful or burning sensation when urinating
Serious Complications
Urinary retention (inability to void) is a serious complication of severe BPH that requires immediate medical attention. Urinary retention can be a sign of obstruction in the bladder. Bladder obstruction can cause kidney damage, bladder stones, urinary tract infections, blood in the urine, and incontinence as urine dribbles out in small amounts.
Diagnosis
A doctor makes a diagnosis of BPH based on description of symptoms, medical history, physical examination, and various blood and urine tests. If necessary, your doctor may refer you to a urologist for more complex test procedures.
Some diagnostic tests are used to rule out cancers of the prostate or bladder as the cause of symptoms. In some cases, symptoms of prostate cancer can be similar to those of BPH. Tests may also be performed to see if BPH has caused any kidney damage.
Medical History
The doctor will ask about your personal and family medical history, including past and present medical conditions. The doctor will also ask about any medications you are taking that could cause urinary problems
Physical Examination
Digital Rectal Exam. The digital rectal exam is used to detect an enlarged prostate. The doctor inserts a gloved and lubricated finger into the patient's rectum and feels the prostate to estimate its size and to detect nodules or tenderness. The exam is quick and painless. The test helps rule out prostate cancer or problems with the muscles in the rectum that might be causing symptoms, but it can underestimate the prostate's size. It is never the sole diagnostic tool for either BPH or prostate cancer.
Other Physical Examinations. The doctor will press and manipulate (palpate) the abdomen and sides to detect signs of kidney or bladder abnormalities. The doctor may test reflexes, sensations, and motor response in the lower body to rule out possible nerve-related (neurologic) causes of bladder dysfunction.
Prostate Specific Antigen (PSA) Test
A PSA test measures the level of prostate-specific antigen (PSA) in the patient's blood. It is a widely used but controversial screening test for prostate cancer. High PSA levels may indicate prostate cancer, but BPH itself usually raises PSA levels. And, some drugs used to treat BPH can decrease PSA levels.
Urinalysis
A urinalysis can detect signs of bleeding or infection. A urinalysis involves a physical and chemical examination of a urine sample. A urinalysis also helps rule out bladder cancer.
Uroflowmetry
To determine whether the bladder is obstructed, an electronic test called uroflowmetry measures the speed of urine flow. To perform this test, the patient urinates into a special toilet equipped with a measuring device. A reduced flow may indicate BPH. However, bladder obstruction can also be caused by other conditions including weak bladder muscles and problems in the urethra.
Cystoscopy
Cystoscopy, also called urethrocystoscopy, is a test performed by a urologist to check for problems in the lower urinary tract, including the urethra and bladder. The doctor can determine the presence of structural problems including enlargement of the prostate, obstruction of the urethra or neck of the bladder, anatomical abnormalities, or bladder stones. The test may also identify bladder cancer, and causes of blood in the urine and infection.
In this procedure, a thin tube with a light at the end (cytoscope) is inserted into the bladder through the urethra. The doctor may insert tiny instruments through the cytoscope to take small tissue samples (biopsies). Cytoscopy is typically performed as an outpatient procedure. The patient may be given local, spinal, or general anesthesia.
Ultrasound
Ultrasound is a painless procedure that can give an accurate picture of the size and shape of the prostate gland. Ultrasound may also be used for detecting kidney damage, tumors, and bladder stones. Ultrasound tests of the prostate generally use one of two methods:
- Transrectal ultrasonography (TRUS) uses a rectal probe for assessing the prostate. TRUS is significantly more accurate for determining prostate volume.
- Transabdominal ultrasonography uses a device placed over the abdomen. It can give an accurate measure of postvoid residual urine and can be used to check for kidney damage caused by severe BPH.
Postvoid Residual Urine
The postvoid residual urine volume (PVR) test measures the amount of urine left after urination. Normally, about 50 mL or less of urine is left; more than 200 mL is a sign of abnormalities. Measurements in between require further tests. The most common method for measuring PVR is with a catheter, a soft tube that is inserted into the urethra within a few minutes of urination.
Ruling Out Other Causes of Symptoms
In addition to prostate cancer, other conditions and factors can cause lower urinary tract symptoms similar to those associated with BPH:
- Structural Abnormalities. Abnormalities in the urinary tract can cause BPH-like symptoms. These abnormalities include narrowing of the urethra, weakened bladder, and prostate muscle contractions. Such conditions can produce obstruction, impair or weaken the detrusor muscle surrounding the bladder, or cause other damage that impacts the urinary tract.
- Prostatitis. Prostatitis is an inflammation of the prostate gland that can be caused by bacterial or nonbacterial factors. (The most common form of prostatitis is nonbacterial, a condition also called prostatosis.) Symptoms include urgent need to urinate, frequent urination, and the need to urinate at night. Pain may occur in the lower back or rectum, or it may develop after ejaculation.
- Medications. Many medications can cause lower urinary tract symptoms or urinary retention, and can worsen symptoms of BPH. These types of medications include antihistamines, decongestants, diuretics, opiates, and tricyclic antidepressants.
Treatment
Because BPH rarely causes serious complications, men usually have a choice between treating it or opting for watchful waiting:
- Watchful Waiting. Watchful waiting (also known as active surveillance) involves lifestyle changes and an annual examination. (Even when choosing watchful waiting, it is important to have a doctor perform an initial examination to rule out other disorders.) BPH is often a progressive condition and if it worsens enough it can cause urinary tract infections, bladder damage, and kidney damage. Your doctor needs to monitor your condition to determine when it may be time to start treatment.
- Treatment. The primary goals of treatment for BPH are to improve urinary flow and to reduce symptoms. Many options are available. They include drug therapies to help shrink or relax the prostate, minimally invasive procedures that use lasers to reduce excess prostate tissue, and surgery to remove part of the prostate.
Deciding Between Treatment and Watchful Waiting
The choice between watchful waiting and treatment usually depends on symptom severity. The American Urological Association’s BPH Symptom Score uses seven questions to evaluate a patient’s urinary symptoms during the past month. (The International Prostate Symptoms Score is another index that is also used.) The questions are:
- How often have you had a sensation of not emptying your bladder completely after you finished urinating?
- How often have you had to urinate again less than 2 hours after you finished urinating?
- How often have you stopped and started again several times when you urinated?
- How often have you found it difficult to urinate?
- How often have you had a weak urinary stream?
- How often had you had to push or strain to begin urination?
- How many times did you most typically get up to urinate from the time you went to bed at night until the time you got up in the morning?
Responses for the first six questions are scaled from “not at all” to “almost always.” (The last question uses answers ranging from “none” to “5 or more times.”) Each response is assigned a number on a scale of 0 - 5 and totaled into a symptom score. The symptom score can fall anywhere between 0 and 35.
Patients with mild symptoms will have low scores and may decide to delay treatment. Higher scores indicate more severe symptoms. Treatment can reduce the score:
- A score reduction of 5 points indicates modest symptom relief
- A score reduction of 5 - 10 points indicates moderate symptom relief
- A score reduction of more than 10 points indicates large symptom relief
Your doctor can discuss with you the various treatment options and the likelihood of symptom relief they may provide. All treatments have various side effects, which need to be taken into consideration. Quality of life is as important as symptom severity.
Treatment Options
Medications. In general, there is no reason to treat BPH with medications unless symptoms become very bothersome. The size of the prostate, determined by exam or ultrasound, cannot indicate the need for medications. Evidence suggests that:
- Medications are the best choice for men with mild-to-moderate symptoms who want treatment. Choices include alpha-blockers, anti-androgens, or a combination of the two. Specific factors indicate the best choice, although most men take an alpha-blocker.
- Men with moderate-to-severe symptoms often respond to the same medications as men with mild symptoms. Recent developments in drug therapy have reduced or delayed the need for surgery.
Surgery. A quarter of men with moderate symptoms, and even more men with severe symptoms, eventually need surgery. If a man chooses surgery, there are many choices. Transurethral resection of the prostate (TURP) is the standard procedure, but less invasive procedures, particularly those using heat or lasers to destroy prostate tissue, are becoming more common.
Click the icon to see an illustrated series detailing transurethral resection of the prostate surgery.
The most common reason for choosing surgery is obstruction of the bladder outlet, which causes urinary retention. Surgery may also be a reasonable option when BPH is clearly related to one or more of the following conditions:
- Recurrent urinary tract infection
- Blood in the urine (hematuria). The drug finasteride may help some men with this condition and should probably be tried before surgery.
- Bladder stones
- Kidney problems
- Moderate-to-severe symptoms that are not well controlled with medications
Increased urinary flow and reduced urine retention are the greatest improvements resulting from surgery. Often, however, the benefits of surgery are not permanent.
Lifestyle Changes
General Lifestyle Recommendations
Certain lifestyle changes may help relieve symptoms and are particularly important for men who choose to avoid surgery or drug therapy. They include:
- Limit daily fluid intake to less than 2,000 mL (about 2 quarts).
- Limit or avoid alcohol and caffeine.
- Limit beverages in the evening. Avoid drinking fluids after your evening meal.
- Try to urinate at least once every 3 hours.
- “Double-voiding” may be helpful -- after urinating, wait and try to urinate again.
- Stay active. Cold weather and immobility may increase the risk for urine retention. Keeping warm and exercising may help.
- Try to achieve and maintain a healthy weight. Obesity and lack of physical activity increase the risk for lower urinary tract symptoms.
Avoiding Medications that Aggravate Symptoms
Decongestants and Antihistamines. Men with BPH should avoid, if possible, the many medications for colds and allergies that contain decongestants, such as pseudoephedrine (Sudafed, generic). Such drugs, known as adrenergics, can worsen urinary symptoms by preventing muscles in the prostate and bladder neck from relaxing to allow urine to flow freely. Antihistamines, such as diphenhydramine (Benadryl, generic), can also slow urine flow in some men with BPH.
Diuretics. Men who are taking diuretics (drugs that increase urination) may want to talk to their doctor about reducing the dosage or switching to another type of drug. Diuretics are important drugs for many people with high blood pressure, with a proven track record for saving lives. No one should go off these medications without medical supervision.
Other Drugs. Other drugs that may worsen symptoms are certain antidepressants and drugs used to treat spasticity.
Pelvic Floor Muscle Training
Pelvic floor muscle exercises, first developed to help women with childbirth, may also help men prevent urine leakage, particularly after surgical procedures. These exercises strengthen the pelvic floor muscles that both support the bladder and close the sphincter.
Performing the Exercises. Since the muscle is internal and sometimes hard to isolate, doctors often recommend practicing while urinating:
- Contract the muscle until the flow of urine is slowed or stopped. He attempts to hold each contraction for 20 seconds.
- Release the contraction.
- In general, patients should perform 5 - 15 contractions, three to five times daily.
Dietary Factors
A heart-healthy diet rich in vegetables and fruit may help reduce BPH risk. Some evidence indicates that fruits and vegetables rich in beta-carotene and vitamin C may help protect against BPH. Dietary choices should also focus on increasing intake of healthy fats, such as omega-3 fatty acids, and limiting intake of unhealthy saturated fats and trans-fatty acids.
Herbs and Supplements
Generally, manufacturers of herbal remedies and dietary supplements do not need approval from the FDA to sell their products. Just like a drug, herbs and supplements can affect the body's chemistry, and therefore have the potential to produce side effects that may be harmful. There have been several reported cases of serious and even lethal side effects from herbal products. Patients should check with their doctor before using any herbal remedies or dietary supplements.
Popular herbal and dietary supplement treatments for BPH include:
- Saw palmetto is one of the most popular herbal remedies for BPH. It comes from the berry of the plant Serenoa repens. Most clinical trials have shown a modest benefit at best. A large, high-quality study found that saw palmetto did not help men with moderate-to-severe BPH when the herb was taken for 1 year. Another high-quality study found that saw palmetto had no benefit even when the dose was tripled.
- Other popular herbs include extracts from African plum tree (Pygeum africanum), rye grass pollen (Secale cerale), stinging nettle root (Urtica dioica), South African star grass (Hypoxis rooperi), and pumpkin seed oil (Cucurbita peponis). Beta-sitosterol is a plant sterol found in some of these herbs that is marketed as a dietary supplement for prostate health. There is no scientific evidence that any of these remedies help treat BPH.
- Patients should be aware that high doses of zinc supplements may increase the risk and progression of BPH.
Medications
The two main drug classes used for BPH are:
- Alpha-blockers. These drugs relax smooth muscles, especially in the bladder neck and prostate. They include terazosin (Hytrin, generic), doxazosin (Cardura, generic), tamsulosin (Flomax, generic), alfuzosin (Uroxatral), and silodosin (Rapaflo). Alpha-blockers help relieve BPH symptoms, but they do not reduce the size of the prostate. The can help improve urine flow and reduce risk of bladder obstruction. They are often the first medication choice, especially for men with smaller prostates.
- 5-alpha-reductase inhibitors. Finasteride (Proscar, generic) and dutasteride (Avodart, Jalyn) block the conversion of testosterone to dihydrotestosterone, the male hormone that stimulates the prostate. These drugs are helpful for men with significantly enlarged prostates. In addition to relieving symptoms, they increase urinary flow and may even help shrink the prostate. However, patients may have to take these drugs for up to 6 - 12 months to achieve full benefits.
Because these two types of drugs work in different ways, combinations of the two may control symptoms in select patients more effectively than either drug alone. The combination treatment may work best for patients with larger prostate glands and higher PSA readings. Many men, however, can control their condition with a single drug.
Alpha-Blockers
Alpha-adrenergic antagonists, commonly called alpha-blockers, relax smooth muscles in the prostate and make it easier for urine to flow. They quickly improve symptoms, usually within days. Because these drugs are short-acting, symptoms return once a man stops taking the medication. Alpha-blockers do not shrink the size of the prostate or change PSA levels.
Alpha-blockers are generally referred to as either nonselective or selective:
- Terzosin (Hytrin, generic) and doxazosin (Cardura, generic) are the nonselective alpha-blockers used for BPH treatment. Nonselective alpha-blockers relax all smooth muscles in the body that surround blood vessels. Because of this, they can lower blood pressure, sometimes causing side effects such as light-headedness or even fainting.
- Tamsulosin (Flomax, Jalyn, generic), alfusozin (Uroxatral), and silodosin (Rapaflo) are the selective alpha-blockers used for BPH. Selective alpha-blockers target more specifically the smooth muscles of the prostate, but they can also affect other areas of the body, such as the eyes. They have fewer side effects than non-selective alpha blockers and are now prescribed much more often than the older drugs.
Side Effects. Alpha-blockers can cause headache, and stuffy or runny nose. Alpha-blockers can reduce blood pressure, which may cause dizziness, lightheadedness, and fainting. Orthostatic hypotension, a sudden drop in blood pressure when standing, can occur and increases the risk of falling. Taking the medication close to bedtime can help reduce these side effects.
Because of the reduced blood pressure side effect, do not take non-selective alpha blockers with the phosphodiesterase (PDE5) inhibitors used for erectile dysfunction [sildenafil (Viagra), tadalafil (Cialis),vardenafil (Levitra), or avanafil (Stendra)]. Men who take selective alpha blockers may be able to use erectile dysfunction pills with guidance from a doctor. (Men may experience a decreased ejaculate while taking these drugs. However, erectile dysfunction is not a usual side effect of alpha-blockers, as it is with finasteride and dutasteride.)
A special concern for tamsulosin, and other selective alpha-blockers, is that they are associated with a condition called intraoperative floppy iris syndrome (IFIS). IFIS is a loss of muscle tone in the iris that can cause complications during cataract surgery. Patients who are planning cataract or other eye surgery should be sure to inform their doctors prior to the surgery. IFIS appears more likely to occur with selective alpha-blockers than non-selective alpha blockers.
5-Alpha-Reductase Inhibitors (5-ARIs)
The prostate gland contains an enzyme called 5 alpha-reductase that converts testosterone to another androgen called dihydrotestosterone. Drugs known as 5-alpha-reductase inhibitors (5-ARIs), block this enzyme and thus reduce dihydrotestosterone in the prostate thereby preventing prostate growth.
The 5-ARIs used for treating BPH are:
- Finasteride (Proscar, generic)
- Dutasteride (Avodart, Jalyn). Jalyn is a 2-in-1 pill that combines dutasteride with the alpha-blocker tamsulosin.
Because 5-ARIs help shrink enlarged prostates, they are most effective in reducing symptoms in men with very large prostates. These drugs take several months before they have an effect so men may not notice any signs of improvement for 3 - 6 months.
Side Effects. Finasteride and dutasteride can cause erectile dysfunction, lowered sexual drive (libido), and ejaculation and orgasm disorders. These drugs can reduce the volume and quality of semen released during ejaculation. These sexual side effects may sometimes persist even after the drug is discontinued. (A positive side effect of finasteride is possible reduction of hair loss related to male hormones and, in some cases, hair growth in men with mild-to-moderate male pattern baldness.)
These drugs decrease prostate-specific antigen (PSA) levels, which may mask the presence of prostate cancer. To resolve this problem, doctors calculate PSA levels in men taking these drugs by doubling the PSA values. This doubling equation helps provide an accurate measurement. The FDA advises doctors that an increase in PSA (even if it’s in a normal range) while taking this drug may indicate the presence of prostate cancer.
A matter of controversial debate is whether 5-ARIs help protect against prostate cancer. Some studies have suggested that 5-ARIs may lower a man’s risk for developing prostate cancer. However, based on other studies, the FDA advises that these drugs may actually increase the risk for being diagnosed with high-grade aggressive types of prostate cancer. At this time, 5-ARIs are not approved for prostate cancer prevention. Men who take these drugs for BPH should discuss this issue with their doctors. The FDA recommends that doctors rule out other urologic conditions, including prostate cancer, that may mimic BPH before prescribing 5-ARIs for BPH treatment.
Other Drugs
Anticholinergic drugs, also called antimuscarinics, such as tolterodine (Detrol) may be helpful for some patients. For treatment of BPH, they may be prescribed either alone or in combination with an alpha-blocker drug.
Tadalafil (Cialis) is approved for treating BPH either alone or when it occurs along with erectile dysfunction. Tadalafil should not be used in combination with alpha-blockers without careful consideration and monitoring for excessive blood pressure lowering. Like all PDE5 inhibitor drugs used for erectile dysfunction, men who take nitrate drugs should not take tadalafil.
Surgery
Several surgical approaches are used to treat BPH. Reasons for performing prostate surgery include:
- Persistent or recurrent episodes of urinary retention (inability to urinate)
- Persistent blood in the urine
- Bladder stones
- Moderate or severe lower urinary tract symptoms that do not improve with medication
Surgical options include invasive and minimally invasive procedures. The choice of which surgical procedure to use depends on various factors, including a man’s age and general health.
The most effective surgical procedure, transurethral resection of the prostate (TURP), is also the most invasive and has the highest risk for serious complications. However, because it is more effective than less invasive procedures, TURP remains the procedure of choice for many doctors.
Minimally invasive procedures use laser or some other form of heat to destroy excess prostate tissue. Although minimally invasive procedures may be an appropriate choice for some patients, including younger men, none to date have proven superior to TURP.
Transurethral Resection of the Prostate (TURP)
Transurethral resection of the prostate (TURP) involves surgical removal of the inner portion of the prostate, where BPH develops. It is the most common surgical procedure for BPH, although the number of procedures has dropped significantly over the past decades because of the increased use of effective medications.
Click the icon to see an illustrated series detailing transurethral resection of the prostate surgery.
Procedure. The surgeon inserts a fiber-optic endoscope, which is a thin tube, into the urethra. No incision or stitches are needed. The surgeon uses the endoscope to cut away excess prostatic tissue, and water solutions are used to flush away the excised matter. TURP usually requires a 1 - 2 day hospital stay.
A Foley catheter generally remains in place for 1 - 3 days after surgery to allow urination. This device is a tube inserted through the opening of the penis to drain the urine into a bag. The catheter can cause temporary bladder spasms that can be painful. The catheter may be removed while the patient is in the hospital or after he is sent home.
Recuperation. Urine flow is stronger almost immediately after most TURP procedures. After the catheter is removed, patients often feel some pain or sense of urgency as the urine passes over the surgical wound. These sensations generally last for about a week and then gradually subside. Complete healing takes about 2 months. The following are some tips for speeding recovery and avoiding complications:
- During recuperation avoid driving, operating heavy equipment, lifting, sudden movements, and straining the muscles in the lower tracts, such as during a bowel movement.
- Drinking 8 glasses of water a day after surgery is important to flush the bladder and help healing.
- Foods that help prevent constipation, such as fruits and vegetables, are important. A laxative may be needed if constipation occurs.
- Pelvic floor exercises can help reduce incontinence. Performing three to four sets of 30 contractions daily is recommended.
- Don’t resume sexual activity until your doctor says it’s safe to do so.
- Check with your doctor about any drugs or herbal supplements that you take to make sure that they will not thin blood and increase bleeding.
Complications. The TURP procedure is generally safe but there are some risks for short- and long-term complications.
Immediate short-term complications after surgery may include:
- Bleeding. Some blood in the urine is normal after TURP surgery but persistent heavy bleeding or clotting is a sign of a more serious complication. In rare cases, if the bleeding is very heavy, patients require blood transfusions.
- Infection. Urinary tract infections are more likely to occur the longer the catheter is in place
- Urination problems. Temporary urinary leaking or dribbling (incontinence) is common after surgery and usually resolves within a month. Temporary urinary retention (inability to urinate) may occur for a few days following surgery (which is why a catheter is used to help remove urine.
- TURP syndrome. If the fluids used during TURP build up, water intoxication can develop, which can be serious. TURP syndrome occurs in a very small percentage of patients and can be treated with diuretics to remove excess fluid.
Long-term complications after surgery may include:
- Retrograde Ejaculation. Retrograde ejaculation, also called dry orgasm is very common. With this condition, the semen is ejaculated into the bladder rather than out through the urethra. Retrograde ejaculation does not affect sexual pleasure but it does impair fertility.
- Erectile Dysfunction. Erectile dysfunction, the inability to maintain an erection, is not common but can occur.
- Urinary Incontinence. Temporary urinary incontinence is common after TURP but in rare cases some men become completely unable to hold back their urine.
- Repeat Surgery. Up to 10% of patients who undergo TURP need a repeat operation within 5 years. Sometimes, scarring in the bladder severe enough to cause obstruction occurs within a year of the procedure and may require transurethral incision (TUIP). More often, the urethra is scarred and narrows, but usually this condition can be corrected by a simple stretching procedure performed in the doctor's office.
Other Invasive Surgical Procedures
Transurethral Incision of the Prostate (TUIP). In TUIP, the surgeon makes only one or two incisions in the prostate, causing the bladder neck and the prostate to spring open and reduce pressure on the urethra. TUIP is generally reserved for men with minimally enlarged prostates (30 grams or less) who have obstruction of the neck of the bladder.
TUIP is less invasive than TURP, has a lower rate of the same complications, particularly retrograde ejaculation, and usually does not require a hospital stay. More studies are still needed, however, to determine whether they are comparative in long-term effectiveness.
Open Prostatectomy. In open prostatectomy, the enlarged prostate is removed through an open incision in the abdomen using standard surgical techniques. This is major surgery and requires a hospital stay of several days. Open prostatectomy is used only for severe cases of BPH, when the prostate is severely enlarged, the bladder is damaged, or other serious problems exist. Some patients need a second operation because of scarring. Side effects of open prostatectomy can include erectile dysfunction and urinary incontinence.
Laser Surgery
Procedures. Laser technology is used for removal of prostate tissue. Laser procedures can usually be done on an outpatient basis, and there is little risk for bleeding. The procedure involves passing a small tube with a tiny camera and the laser fiber through the urethra of the penis. The procedure is performed under spinal, epidural, or general anesthesia.
Laser procedures have a faster recovery time and less risk of incontinence than invasive surgical procedures, but their long-term effectiveness is unclear. Laser surgery may not be appropriate for men with larger prostates. Different procedures are used to provide different degrees of thermal cell destruction that range from coagulation to complete vaporization:
- Transurethral holmium laser ablation of the prostate (HoLAP) uses laser energy to target and vaporize obstructing prostate tissue. The removal of the tissue helps to restore urine flow.
- Transurethral holmium laser enucleation of the prostate (HoLEP) is similar to HoLAP except a portion of the prostate is cut into smaller pieces and then flushed out from the bladder.
- Holmium laser resection of the prostate (HoLRP) is similar to HoLEP except the prostate fragments are removed through a resectoscope instrument.
- Photoselective vaporization of the prostate (PVP) uses a potassium-titanyl-phosphate (KTP) laser ("green-light" laser) to vaporize prostate tissue. The procedure is virtually bloodless and may be a better option for men taking anticoagulant ("blood thinner") medication. Improvement lasts for up to 1 year after the procedure. More studies are needed to confirm long-term efficacy.
Other Less Invasive Procedures
These minimally invasive procedures carry fewer risks for incontinence or problems with sexual function than invasive procedures, but it is unclear how effective they are in the long term.
Transurethral Microwave Thermotherapy (TUMT). Transurethral microwave thermotherapy delivers heat using microwave pulses to destroy prostate tissue. A microwave antenna is inserted through the urethra with ultrasound used to position it accurately. The antenna is enclosed in a cooling tube to protect the lining of the urethra. Computer-generated microwaves pulse through the antenna to heat and destroy prostate tissue. When the temperature becomes too high, the computer shuts down the heat and resumes treatment when a safe level has been reached. The procedure takes 30 minutes to 2 hours, and the patient can go home immediately afterward.
Transurethral Needle Ablation (TUNA). Transurethral needle ablation is a relatively simple and safe procedure, using needles to deliver high-frequency radio waves to heat and destroy prostate tissue.
Transurethral Electrovaporization (TUVP). Transurethral electrovaporization uses high voltage electrical current delivered through a resectoscope to combine vaporization of prostate tissue and coagulation that seals the blood and lymph vessels around the area. Deprived of blood, the excess tissue dies and is sloughed off over time.
Prostatic Stents
Prostatic stents used for BPH are flexible mesh tubes that are inserted into the urethra. Typically, the insertion procedure takes only 15 minutes. Patients need only regional anesthetic and mild sedation. There is minimal recuperation and no overnight hospital stay. Unfortunately, stents often need to be removed later because of poor placement or complications, including irritation when urinating, urinary tract infections, and treatment failure. At this point, stents seem best suited for high-risk surgical patients or those with a limited life expectancy.
Resources
- www2.niddk.nih.gov -- National Institute of Diabetes and Digestive and Kidney Diseases
- www.auanet.org -- American Urological Association
References
Abrams P, Chapple C, Khoury S, Roehrborn C, de la Rosette J; International Scientific Committee. Evaluation and treatment of lower urinary tract symptoms in older men. J Urol. 2009 Apr;181(4):1779-87. Epub 2009 Feb 23.
Auffenberg GB, Helfand BT, McVary KT. Established medical therapy for benign prostatic hyperplasia. Urol Clin North Am. 2009 Nov;36(4):443-59, v-vi.
Barry MJ, Meleth S, Lee JY, Kreder KJ, Avins AL, Nickel JC, et al. Effect of increasing doses of saw palmetto extract on lower urinary tract symptoms: a randomized trial. JAMA. 2011 Sep 28;306(12):1344-51.
Bell CM, Hatch WV, Fischer HD, Cernat G, Paterson JM, Gruneir A, et al. Association between tamsulosin and serious ophthalmic adverse events in older men following cataract surgery. JAMA. 2009 May 20;301(19):1991-6.
Burke N, Whelan JP, Goeree L, Hopkins RB, Campbell K, Goeree R, et al. Systematic review and meta-analysis of transurethral resection of the prostate versus minimally invasive procedures for the treatment of benign prostatic obstruction. Urology. 2010 May;75(5):1015-22. Epub 2009 Oct 24.
Davidson JH, Chutka DS. Benign prostatic hyperplasia: treat or wait? J Fam Pract. 2008 Jul;57(7):454-63.
Donnell RF. Minimally invasive therapy of lower urinary tract symptoms. Urol Clin North Am. 2009 Nov;36(4):497-509, vi-vii.
Kramer BS, Hagerty KL, Justman S, Somerfield MR, Albertsen PC, Blot WJ,et al. Use of 5-alpha-reductase inhibitors for prostate cancer chemoprevention: American Society of Clinical Oncology/American Urological Association 2008 Clinical Practice Guideline. J Clin Oncol. 2009 Mar 20;27(9):1502-16. Epub 2009 Feb 24.
Lourenco T, Pickard R, Vale L, Grant A, Fraser C, MacLennan G, et al. Minimally invasive treatments for benign prostatic enlargement: systematic review of randomised controlled trials. BMJ. 2008 Oct 9;337:a1662. doi: 10.1136/bmj.a1662.
McVary KT, Roehrborn CG, Avins AL, Barry MJ, Bruskewitz RC, Donnell RF, et al. Update on AUA guideline on the management of benign prostatic hyperplasia. J Urol. 2011 May;185(5):1793-803. Epub 2011 Mar 21.
Moyad MA, Lowe FC. Educating patients about lifestyle modifications for prostate health. Am J Med. 2008 Aug;121(8 Suppl 2):S34-42.
Penson DF, Munro HM, Signorello LB, Blot WJ, Fowke JH; Urologic Diseases in America Project. Obesity, physical activity and lower urinary tract symptoms: results from the Southern Community Cohort Study. J Urol. 2011 Dec;186(6):2316-22. Epub 2011 Oct 20.
Roehrborn CG. Male lower urinary tract symptoms (LUTS) and benign prostatic hyperplasia (BPH). Med Clin North Am. 2011 Jan;95(1):87-100.
Roehrborn CG, Siami P, Barkin J, Damião R, Major-Walker K, Morrill B, et al. The effects of dutasteride, tamsulosin and combination therapy on lower urinary tract symptoms in men with benign prostatic hyperplasia and prostatic enlargement: 2-year results from the CombAT study. J Urol. 2008 Feb;179(2):616-21; discussion 621. Epub 2007 Dec 21.
Sarma AV, Wei JT. Clinical practice. Benign prostatic hyperplasia and lower urinary tract symptoms. N Engl J Med. 2012 Jul 19;367(3):248-57.
Tacklind J, Fink HA, Macdonald R, Rutks I, Wilt TJ. Finasteride for benign prostatic hyperplasia. Cochrane Database Syst Rev. 2010 Oct 6;(10):CD006015.
Theoret MR, Ning YM, Zhang JJ, Justice R, Keegan P, Pazdur R. The risks and benefits of 5a-reductase inhibitors for prostate-cancer prevention. N Engl J Med. 2011 Jun 15. [Epub ahead of print].
|
Review Date:
9/19/2012 Reviewed By: Harvey Simon, MD, Editor-in-Chief, Associate Professor of Medicine, Harvard Medical School; Physician, Massachusetts General Hospital. Also reviewed by David Zieve, MD, MHA, Medical Director, A.D.A.M. Health Solutions, Ebix, Inc. |





